Green Libraries Week – Climate Crisis Eresources

Throughout Green Libraries Week, we’ve been blogging about the relationship between sustainability and libraries, and highlighting LSHTM Library resources and initiatives. As noted in the introductory post on Monday, the climate crisis can affect and is affecting every one of us, while particularly affecting many of the world’s most vulnerable communities. LSHTM Library collects resources on climatology, climate change, and sustainability as they are important to public health and global health. Monday’s blogpost also highlighted some of the physical books on the topic that we have in our collections, which area also currently on display in the Library ready for you to browse at your convenience. This post seeks to build on that, by highlighting some of our other resources on sustainability and climate change, such as databases, ebooks, or journal collections.
Journals
The Library subscribes to JSTOR’s Sustainability Collection. This consists of numerous journals – more than 100 at last count – and research reports from thinktanks worldwide, tackling the topic of sustainability from a huge variety of angles and perspectives. From journals focused on sociology, law, or organisations, like Urban Studies, Renewable Energy Law and Policy Review, or Journal of Asian Sociology, to those dealing with climatology, agriculture, or engineering, such as Journal of Hydrometeorology, Renewable Agriculture and Food Systems, or Wind Engineering. Take a look at JSTOR’s own web guide for even more details, and have a look around for yourself on the site!
In addition to all these resources, the Library has catalogued materials from free and Open Access journals, including many related to climate change, sustainability, and environmental sciences in general. You’ll therefore be able to find relevant open access articles for your research in these areas just by searching our catalogue. You can also search for and browse for journals on the DOAJ (Directory of Open Access Journals). Linked on there are currently 95 more journals related to climate change.
Databases
Performing a literature search rather than browsing around for reading material? Not to worry – in addition to larger databases covering all aspects of science, we can also signpost you to several databases specialising in environmental and climate research. For instance, REPIDISCA is a regional portal for data from UN agencies relating to sanitary engineering and environmental sciences in Latin America and the Caribbean. GreenFILE, on the other hand, covers any area related to the environment’s relationship with humans, including sustainability, climate change, and pollution.
Our Databases page also lets you filter all of the databases we subscribe to by subject matter, including environmental health.
eBooks
We have access to numerous climate studies and sustainability ebooks, such as
- FitzRoy, Felix, and Elissaios Papyrakis. An Introduction to Climate Change Economics and Policy.
- Friel, Sharon. Climate Change and the People’s Health.
- Gaard, Greta Claire. Critical Ecofeminism.
- Mann, Michael E. The New Climate War : the Fight to Take Back the Planet.
- McMichael, A. J. Human Frontiers, Environments, and Disease : Past Patterns, Uncertain Futures.
Open Access ebooks accessible by searching the Library include:
- The Hindu Kush Himalaya Assessment: Mountains, Climate Change, Sustainability and People.
- Negotiating Climate Change in Crisis.
- Swilling, Mark. The Age of Sustainability: Just Transitions in a Complex World.
- Vincenzo Dovì (Ed.), and Antonella Battaglini (Ed.). Energy Policy and Climate Change.
Try searching Discover for keywords like ‘sustainability’ or ‘climate change’ to find even more resources. You can also filter results to only include books, or narrow down dates of publication, or a variety of other options. Make sure you’re logged into Discover when searching it, so you can access all available information and really get the most out of your searches.
Green Libraries Week – Recycling

“Recycling cuts carbon dioxide emissions by 700 million tonnes a year. Recycling is one of the solutions to combat climate change. Recycling reduces the need to use new natural resources, including the fossil fuels that are used to make most plastics. For every tonne of paper recycled, for example, 17 trees can be saved and water used in manufacturing is cut by 50%.
It is estimated that recycling has the potential to reduce carbon emissions by the equivalent of 10.4-11.2 Gt of carbon dioxide equivalent (CO2e) emissions between 2020-2050, which would be equivalent to the amount of carbon dioxide Japan emits in a year”. How recycling can help the climate and other facts – BBC Future
LSHTM provide recycling bins for general waste and recyclable items such as newspapers, cans etc. All of the printers at LSHTM use recycled paper. We also recycle waste generated by the printers and have recently introduced a battery recycling point. As part of our collections policy, print material intended for disposal is passed to a bookseller for reuse as a sustainable solution. The move towards online journal subscriptions as opposed to print also reduces paper consumption.
The library holds an online subscription to Recycling.
Green Libraries Week – Energy Use and Waste Reduction
Acting sustainably as a university library is about reducing consumption of resources where possible, and reducing wasted resources through reuse. We’ve already explored the importance of acting sustainably with regard to water yesterday in another blogpost. Energy is another resource we need to use carefully, especially while universities are still transitioning to fully renewable energy sources.
From heating, lighting, to IT equipment, some energy use by libraries is inevitable. However, there are energy-saving measures that are both achievable and which add up to have an effect. These include powering off unused devices, motion sensors on lights and printers, and reusing materials like paper where possible. For example, a 2020 article in the journal Sustainability estimated that a university building using motion detectors could save 32.4% of the energy used to light its lecture theatres.
At LSHTM as a whole, motion sensors have been installed in the majority of common areas and offices, including much of the Library. Printers are also fitted with motion sensors so that they can save power. Within the Library, unused devices are powered down and resources like paper and office supplies are reused by staff as much as possible. Of course, there’s always more that can be done and is planned to be done – many of the aims in LSHTM’s plans to reach net zero by 2030 will also contribute to saving energy.
Library resources on energy and sustainability
The Library also holds lots of resources on sustainable management of resources. Have a look at some of these, for starters:
- Bongartz, Petra, Naomi Vernon, and John Fox, eds. Sustainable Sanitation for All: Experiences, Challenges, and Innovations. Rugby, Warwickshire, UK: Practical Action Publishing Ltd, 2016. Print.
- Dannenberg, Andrew L., and Howard Frumkin. Making Healthy Places: Designing and Building for Health, Well-Being, and Sustainability. Washington, DC [u.a: Island Press, 2011. Print.
- Jastrup, Morten., and Marie. Drique. Buildings: Exploring the Sustainable Buildings of Tomorrow. Copenhagen: Monday Morning, 2013. Print.
- Consumption, Sustainability and Everyday Life. Cham: Springer Nature, 2023. Web.
- Sustainability in Urban Planning and Design. N.p., 2020. Web.
- Hyysalo, Sampsa. Citizen Activities in Energy Transition: User Innovation, New Communities, and the Shaping of a Sustainable Future. Taylor & Francis, 2021. Web.
- Energy Transition in the Baltic Sea Region: Understanding Stakeholder Engagement and Community Acceptance. Taylor & Francis, 2022. Web.
- Electricity Access, Decarbonization, and Integration of Renewables: Insights and Lessons from the Energy Transformation in Bangladesh, South Asia, and Sub-Sahara Africa. Wiesbaden: Springer Nature, 2023. Web.
- Lovell, Heather. Understanding Energy Innovation: Learning from Smart Grid Experiments. Bern: Springer Nature, 2022. Web.
Green Libraries Week – Water Sustainability

Water is at the core of sustainable development and is critical for socio-economic development, healthy ecosystems and for human survival itself. Its judicious management is a prerequisite for sustainable development.
In the last 15 years, consumption of bottled water has doubled. Along with an increase in consumption of other soft drinks, this means 13 billion plastic bottles are now used in the UK every year. Plastic bottles make up one third of all plastic pollution in the sea, and there are now over 159 plastic bottles for every mile of beach in the UK. http://www.refill.org Encouraging people to carry and refill a reusable bottle, and making it easy for them to do so – such as by providing drinking water fountains – is one of the most effective ways to reduce plastic pollution at source. According to research by Keep Britain Tidy and BRITA, 78% of people say they would like to see greater availability of free tap water in public spaces. Water fountains provide an accessible and convenient way for people to refill bottles and drink tap water on the go.
LSHTM library is in the process of replacing our water cooler bottles with water fountains sourced from the mains water supply.
In our collection we hold a number of titles on water and sustainability. A selection are as follows:
Garrick, Dustin E. ; Hall, Jim W. ; Dobson, Andrew ; Damania, Richard ; Grafton, R. Quentin ; Hope, Robert ; Hepburn, Cameron ; Bark, Rosalind ; Boltz, Frederick ; De Stefano, Lucia ; O’Donnell, Erin ; Matthews, Nathanial ; Money, Alex (2017), Valuing Water for Sustainable Development. Science, Vol.358 (6366), p.1003-1005.
Gjorgievski, Vladimir Z. ; Markovska, Natasa ; Pukšec, Tomislav ; Duić, Neven ; Foley, Aoife (2021), Supporting the 2030 agenda for sustainable development: Special issue dedicated to the conference on sustainable development of energy, water and environment systems 2019, Renewable & sustainable energy reviews, Vol.143, p.110920, Article 110920
Ongley E.D. United Nations. Economic and Social Commission for Asia and the Pacific (1997), Guidelines on water and sustainable development : principles and policy options
Singh, Katar; Balooni, Kulbhushan ; Venkatachalam, L (2016), Managing Water for Sustainable Development: an Economist’s Perspective, IIM Kozhikode society & management review, Vol.5 (1), p.1-4
Tsani, Stella ; Koundouri, Phoebe ; Akinsete, Ebun (2020) Resource management and sustainable development: A review of the European water policies in accordance with the United Nations Sustainable Development Goals. Environmental science & policy, Vol.114, p.570-579.
UNESCO (2020) Climate Change, Water and Sustainable Development. The United Nations World Water Development Report. p.30-37
02 – 08 October 2023 is Green Libraries Week
Every year Libraries Week celebrates the contribution that libraries have to offer their communities across the UK. Libraries Week is organised by the library and information association, CILIP and the theme this year is climate change and sustainability:
“In 2023, Libraries Week becomes Green Libraries Week, a celebration of the transformative role of libraries and information services in all sectors to address sustainability and climate change.” (Source: CILIP, Libraries Week. accessed: 25 September 2023).
The rapid change in our climate, mainly caused by unsustainable human activity such as the burning of fossil fuels, is causing extreme weather conditions across the planet. This can impact severely on more vulnerable populations, exacerbating existing inequalities:
“Climate change can affect our health, ability to grow food, housing, safety and work. Some of us are already more vulnerable to climate impacts, such as people living in small island nations and other developing countries. Conditions like sea-level rise and saltwater intrusion have advanced to the point where whole communities have had to relocate, and protracted droughts are putting people at risk of famine. In the future, the number of “climate refugees” is expected to rise.” (Source: United Nations. What Is Climate Change? accessed: 25 September 2023).
Although solutions are needed on a global level, libraries have their own part to play by by putting environmental impact and sustainability as an integral part of the planning and delivery of their services, for example. recycling waste, using ethical suppliers etc.
During Green Libraries Week we will be putting out a series of short blogs highlighting a few of the measures we have already put in place in our own library with sustainability and climate change in mind.
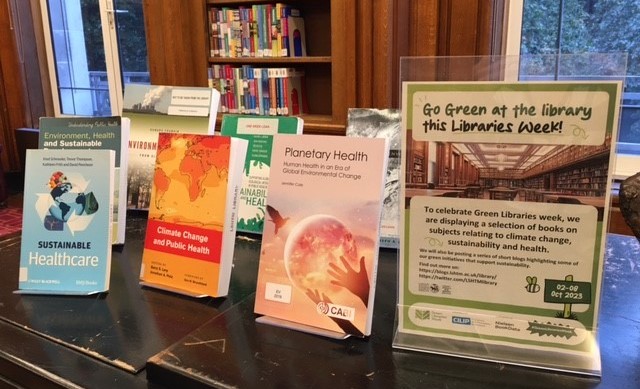
There is also a book display in our main reading room showing a selection of titles in our collections on subjects relating to climate change and sustainability. You can search our collections and resources using our search tool Discover.
See what is going on during Green Libraries Week by following @librariesweek on Twitter/”X”.
(Featured image courtesy of: https://librariesweek.org.uk/libraries-hub/logos/).
Further resources:
https://www.cilip.org.uk/page/GreenLibraries
https://www.un.org/sustainabledevelopment/climate-change/
Books on Display:
Sasser, Jade. On Infertile Ground: Population Control and Women’s Rights in the Era of Climate Change. New York: New York University Press, 2018.
Hutchinson, Emma, and Sari Kovats, eds. Environment, Health and Sustainable Development. Second edition. London: Open University Press, 2016.
Frumkin, Howard, ed. Environmental Health: from Global to Local. Third edition. San Francisco: Jossey Bass, 2016.
Schroeder, Knut. Sustainable Healthcare. Chichester, West Sussex: John Wiley & Sons, 2013.
Des Jardins, Joseph R. Environmental Ethics: an Introduction to Environmental Philosophy. 3rd ed. Belmont, CA: Wadsworth Thomson Learning, 2000.
Brown, Valerie A. Sustainability and Health: Supporting Global Ecological Integrity in Public Health. London: Earthscan, 2005.
FitzRoy, Felix, and Elissaios Papyrakis. An Introduction to Climate Change Economics and Policy. London; Sterling, VA: Earthscan, 2010.
Cole, Jennifer. Planetary Health: Human Health in an Era of Global Environmental Change. Oxfordshire, UK ; Boston, MA: CABI, 2019.
Levy, Barry S., and Jonathan Patz, eds. Climate Change and Public Health. Oxford; New York: Oxford University Press, 2015.
Butler, Colin D. Climate Change and Global Health. Wallingford, Oxfordshire; Boston, MA: CABI, 2014.
The Anatomy of a Silent Crisis. Geneva: Global Humanitarian Forum, 2009.
Bodansky, Daniel, Jutta Brunnée, and Lavanya Rajamani. International Climate Change Law. Oxford: Oxford University Press, 2017.
Griffiths, Jenny. The Health Practitioner’s Guide to Climate Change: Diagnosis and Cure. London; Sterling, Va.: Earthscan, 2009.
Coutts, Christopher. Green Infrastructure and Public Health. Abingdon, Oxon: Routledge, 2015.
Yap, Christopher. Thinking Beyond Sectors for Sustainable Development. Ed. Jeff. Waage and Christopher Yap. Place of publication not identified: Ubiquity Press Ltd, 2015.
ICEH Announces New Public Eye Health Clinical Fellows
[et_pb_section fb_built=”1″ _builder_version=”4.16″ _module_preset=”b0e4c9b5-961b-40ec-ac55-8f48db86eca9″ custom_padding=”||4px|||” global_colors_info=”{}” theme_builder_area=”post_content”][et_pb_row _builder_version=”4.16″ _module_preset=”6996170d-642c-4a52-9572-9cc26dbfecf7″ background_size=”initial” background_position=”top_left” background_repeat=”repeat” global_colors_info=”{}” theme_builder_area=”post_content”][et_pb_column type=”4_4″ _builder_version=”4.16″ _module_preset=”default” custom_padding=”|||” global_colors_info=”{}” custom_padding__hover=”|||” theme_builder_area=”post_content”][et_pb_text _builder_version=”4.18.0″ _module_preset=”default” link_text_color=”#0c71c3″ background_size=”initial” background_position=”top_left” background_repeat=”repeat” custom_margin=”-50px|||||” custom_padding=”||0px|||” hover_enabled=”0″ global_colors_info=”{}” theme_builder_area=”post_content” sticky_enabled=”0″]
© Nick Burn / CBM
Earlier this year the International Centre for Eye Health, in conjunction with the LV Prasad Eye Institute (LVPEI) and the Fred Hollows Foundation announced an 18-month fellowship training programme to strengthen individual capacity in public health and clinical skills.
We are now able to announce the awardees of this inaugural fellowship, which focuses on comprehensive ophthalmology and includes mentorship and a clinical placement in India as part of the course.
The 2023 fellows are:
Dr Gladys Atto, Uganda
“Since graduating in 2018, I have been working in Karamoja subregion, a hard-to-reach area in Uganda with a population of about 1.2 million people as the first and only ophthalmologist. This fellowship comes in handy to equip me with the necessary clinical skills, an opportunity I dearly miss because of working alone. I am confident that the fellowship will not only enhance my skills in comprehensive management of eye patients and public eye health but provide me with the opportunity of networking with various senior ophthalmologists.”
Dr Brenda Walaba, Kenya
“I am an ophthalmologist with slightly more than 4 years of experience as a consultant working at Mbagathi hospital in Nairobi. This is a government institution in the capital city of Kenya. I also double up as the chief county ophthalmologist where I oversee provision of affordable eye health services to more than 4 million Kenyans living in Nairobi city, most of them being from the low socio-economic status.
I was motivated to pursue the Global eye health and clinical fellowship programme after seeing the need in the city of Nairobi where there is a huge population that cannot access affordable and quality eye health services due to high costs. There has also been a rise in patients losing their sight due to cataracts, glaucoma and ocular complications of systemic diseases like Diabetes and Hypertension.
Working in a government hospital where these services are subsidized, I am excited that this fellowship will equip me with the knowledge and skills that I require to reach out to this vulnerable population.”
Dr Beatrice Monday Bako, Uganda
“The fellowship is a great opportunity to improve on my skills and knowledge in the field. It is great idea to offer this opportunity to many more young ophthalmologists to be able to address global visual impairment.”[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]
Library Inductions for new students 2023/24 – Welcome to LSHTM!
A very warm welcome to all those starting this week! It was great to meet so many of you at the Welcome Fair today 🙌
To help you get started using our resources and services, we hope you can attend one of our Induction sessions.
Next week (Week 1) we’re offering sessions Monday to Friday, at lunchtime and in the evening.
Library Induction: using the Library, finding and accessing resources
Monday 02 October – 13:00-14:00 / 17:30-18:30
Tuesday 03 October – 13:00-14:00 / 17:30-18:30
Thursday 05 October – 13:00-14:00 / 17:30-18:30
Friday 06 October – 13:00-14:00 / 17:30-18:30
(Kindly note that sessions which were due to take place on Wednesday 04 October have unfortunately had to be cancelled due to transport disruption on National Rail and TfL services. You are also advised to check before you start your journey if you are planning to travel in to use the Library on that day.)
As space is limited, we ask that you kindly book a place in advance.
How to book on a session:
1. go to the Library Moodle page: tinyurl.com/ismoodle
2. Scroll down to the section headed “Information for MSc students 2023-24” on the Library Moodle page and use the booking link.
3. Book your preferred session. Then just turn up on the day!
The session will give you an introduction to the Library services, help you understand your reading list, and ensure you’re ready to find and access books, journals, articles and databases at LSHTM.
It is aimed at Masters-level students, but anybody is welcome to attend.
The class will also be delivered live using Zoom during the week beginning 16 October. There will be more information to come about these sessions next week.
We look forward to seeing you in the Library soon and supporting you in your studies this year.
Library Inductions for new students.
A very warm welcome to all those starting this week! It was great to meet so many of you at the Welcome Fair today.
To help you get started using our resources and services, we hope you can attend one of our Induction sessions.
Next week (Week 1) we’re offering sessions Monday to Friday, at lunchtime and in the evening.
Library Induction: using the Library, finding and accessing resources
Monday 02 October – Friday 06 October
1:00pm-2:00pm and 5:30pm-6:30pm
(NB – you only need to book one session.)
As space is limited, we ask that you kindly book a place in advance.
How to book on a session:
1. go to the Library Moodle page: tinyurl.com/ismoodle
2. Scroll down to the section headed “Attention NEW MSc students 2023-24” on the Library Moodle page and use the booking link.
3. Book your preferred session. Then just turn up on the day!
The session will give you an introduction to the Library services, help you understand your reading list, and ensure you’re ready to find and access books, journals, articles and databases at LSHTM.
It is aimed at Masters-level students, but anybody is welcome to attend.
The class will also be delivered live using Zoom during the week beginning 16 October. There will be more information to come about these sessions next week.
We look forward to seeing you in the Library soon and supporting you in your studies this year.

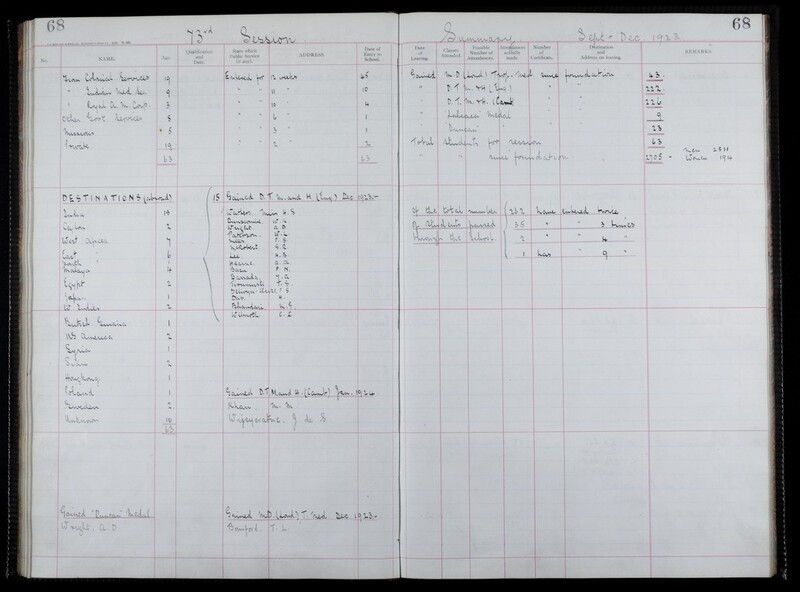
Class of 1923
As we welcome new students to the London School of Hygiene & Tropical Medicine, it seems appropriate that we reflect on the students who attended 100 years ago, the class of 1923.
The 73rd session ran from September to December. 63 students attended the School, of these 57 were men and 6 were women. They came from the following services:
- Colonial Service: 19
- Indian Medical Service: 9
- Royal Army Medical Corps: 3
- Other Government Service: 3
- Missions: 5
- Private: 19
The School’s student registers record a number of details about the students including their destination on leaving, the majority of students went to Asia (28), and the next most popular destination were countries in Africa (16) but students ended up all over the world including Europe, West Indies and America. Unfortunately there is no group photo of this session.
As is shown, many of the students came from the Colonial Service and went on to work in British Colonies. LSHTM has recently published LSHTM and Colonialism – A report on the Colonial History of the London School of Hygiene & Tropical Medicine (1899 – c.1960) which provides a detailed account of our colonial origins and its legacy. LSHTM was set up as a colonial institution and benefitted from and contributed to British colonialism in a variety of ways between 1899 and 1960. It is largely to its role in British colonialism that the LSHTM owes its current power and position as a leader in health research and teaching.
The LSHTM Archives Service is re-examining the collections we hold, the stories we tell and the role we play in critically engaging with the School’s colonial legacy. We have developed a set of principles for decolonising the archive which we are incorporating into our daily working practice.
Students undertook a 12 week course and which cost £21 (£1326.22 in today’s money). Students had to be qualified medical practitioners of any nationality or sex or be in the fifth year of their medical studies. The School Committee had the power, at their discretion, to admit other applicants under special circumstances. Students were asked to bring their own microscopes, with slides and cover glasses, the School provided stains, chemical reagents and pathological material.
Students were taught by a variety of lecturers on tropical diseases including malaria, blackwater fever, trypanosomiasis, yellow fever, leishmaniasis, filariasis, dysentery, pellagra, beri-beri, cholera, plague, dengue, leprosy and eye diseases.
The prospectus for 1923 also lists exams questions from the previous session which included:
- Write a short essay on the extraction of the teeth.
- A small town is reported to be ‘very malarious’. What investigations would you make with a view to measuring the amount of infection amongst the population?
- Identify the snake exhibited and state briefly the symptoms like to follow an effective bite from such a snake
- Describe the operation of ‘evisceration of the eyeball’. Under what circumstances would you recommend the operation?
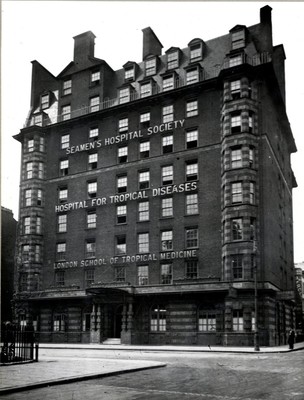
The students were taught in Endsleigh Gardens, this was a former hotel that was converted to a hospital for officers during the First World War and was suitably equipped to house both the Hospital for Tropical Diseases and the School. This building is still standing in Gordon Street and is now the student union for University College London. The School moved from its original home in the Albert Docks in early 1920, although the building wasn’t officially opened until November 1920. The School remained here until 1929 when we moved to the Keppel Street site.
There was a link with Keppel Street as some of the students lived in the Indian YMCA which was on the Keppel Street site. In August 1916 a wooden mock-Tudor YMCA Hut opened on the corner of Keppel and Gower Street in London’s Bloomsbury. “The Shakespeare Hut” as it was called became a home from home for predominantly Anzac soldiers on leave from the Front and remained so until 1919 when it housed the Indian YMCA for three years before it was pulled down in 1920s to make way eventually for the London School of Hygiene & Tropical Medicine which still occupies this site today.
For further information on the history of LSHTM, please contact archives@lshtm.ac.uk
Artificial Intelligence for Diabetic Retinopathy in LMICs: The Research So Far
Image: © Ashley Gilbertson / Commonwealth Eye Health Consortium
Artificial intelligence (AI) has the potential to revolutionise many areas of healthcare. Alongside improving healthcare in high income countries, it promises rapid gains in low- and middle-income countries (LMICs), where AI tools can reduce the need for skilled clinical staff, especially in remote locations.
Despite this promise, implementation into health systems is so far limited. Ophthalmology is a speciality that could particularly benefit from AI, and within eye health diabetic retinopathy (DR) is a disease that shows great potential for AI tools.
DR is a common complication of diabetes and is a leading cause of blindness globally. Early screening and treatment can substantially reduce the risk of sight loss in people with the disease. By submitting retinal photographs from people with diabetes to an AI tool, grading of DR, where the severity of the disease is assessed, can be automated. This can reduce the burden on specialist eye care staff and streamline referrals to other services by providing a diagnosis at the point of screening.
To ascertain the progress of this new technology in low-income settings, and identify areas for future research, a new study by ICEH looked at how AI has been used for DR in LMICs.
The review article included 81 papers. Most of these focused on the performance of AI tools for interpreting retinal photos and providing a grade. Others had different specific outcomes such as grading other retinal conditions at the same time, or looking at macular oedema, a swelling of the retina that can be caused by different diseases, including diabetes.
The authors found that the majority of papers reported how accurate the AI tools were for detecting and grading retinal images for DR, with promising results. However, there was limited evidence for the implementation of these tools into clinics and whether they led to improvements in eye health services or patients’ vision.
Only three of the studies looked at whether and how an AI tool could be successfully implemented into clinical services. A number of challenges were noted including issues such as electricity and internet access. One of these studies from Rwanda showed that when AI-assisted DR screening was combined with a referral decision on the day, the proportion of people attending the specialist eye clinic was increased, indicating the value of a point-of-screening result.
Nearly two thirds of studies came from India, China and Thailand, all middle-income countries, highlighting a lack of research in low-income settings. If this trend continues it could lead a widening of the digital health divide.
None of the studies looked at different AI tools on the same dataset, making it difficult to make a meaningful comparison between different systems.
Furthermore, other crucial factors such as information on regulatory approvals and the cost of using the AI tools were not easily available. Other considerations include legal and ethical issues, which are important for data storage and accountability for errors. Improved screening also needs to be coupled with improved access to treatment for DR, the authors note.
Overall, the study highlights the significant potential for AI to improve diabetic eye care in LMICs. However, there is a need for more studies to evaluate the impact of AI on eye health programmes and visual outcomes. If AI can be shown to improve outcomes in low-income countries whilst being integrated appropriately and cost-effectively into existing health systems, it will be a valuable technology to improve and strengthen eye care.
Publication
Cleland CR, Rwiza J, Evans JR et al. Artificial intelligence for diabetic retinopathy in low-income and middle-income countries: a scoping review. BMJ Open Diabetes Research & Care. August 2023. https://doi.org/10.1136/bmjdrc-2023-003424
[/et_pb_text][/et_pb_column][/et_pb_row][/et_pb_section]