By Kjell Arne Johansson (University of Bergen) Kirsten Bjerkreim Strand (University of Bergen), Abebaw Fekadu (Addis Ababa University) and Dan Chisholm (World Health Organization)
This blog is published as a policy brief here: http://www.uib.no/en/rg/globpri
Mental and neurological health care has long been neglected in low-income settings. This is a blog on an article that was published in Health Policy and Planning: “Health Gains and Financial Protection Provided by the Ethiopian Mental Health Strategy: an Extended Cost-Effectiveness Analysis” on 10th October, World Mental Health Day 2016.
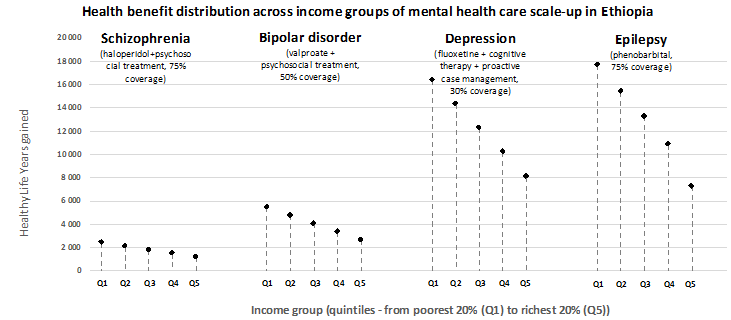
The Ethiopian mental health policy is ambitious and essential treatments for depression, bipolar disorder, schizophrenia and epilepsy are aimed to be scaled-up in all primary care levels. This study was conducted in Ethiopia because there is a need for equity relevant evidence for priority setting on the path to universal health care. Around 155,000 healthy life years can be gained and the poorest are expected to gain the most. In addition, scale-up of psychological therapy and antidepressants are expected to give US$ 50 million in return to the US$ 65 million investments because the working population will be more productive when not depressed.
This paper estimates health and non-health impacts of fully publicly financed care for selected key interventions in the National Mental Health Strategy in Ethiopia. This policy aims to provide essential mental health care at a primary health centre level and to make such services available to a large proportion of those in need.
A methodology of Extended Cost-Effectiveness Analysis (ECEA) was applied to mental and neurological health care in Ethiopia. The impact of providing a package of selected interventions free of charge in Ethiopia was estimated for:
Epilepsy: 75% coverage, phenobarbital
Depression: 30% coverage, fluoxetine, cognitive therapy and proactive case management
Bipolar affective disorder: 50% coverage, valproate and psychosocial therapy
Schizophrenia: 75% coverage, haloperidol plus psychosocial treatment).
Multiple outcomes are estimated:
- healthy-life-years gained
- household out-of-pocket expenditures averted
- expected financial risk protection
- productivity impact
The expected total benefits for the whole population in Ethiopia were evaluated. In addition, we evaluated the expected distribution of benefits across income groups – if policy targets are achieved.
Main findings
(1) The National Mental Health Strategy in Ethiopia for depression, bipolar disorder, schizophrenia and epilepsy is estimated to cost equivalent to US$ 1.8 per capita (US$ 177 million) and to yield large progressive health benefits (see illustration above)
(2) In total, the National Mental Health Strategy is expected to gain 155,000 healthy life years. Divided into disease categories, the benefits (and costs) are:
– Epilepsy: 64,500 healthy life years (US$37m)
– Depression: 61,300 healthy life years (US$65m)
– Bipolar disorder: 20,300 healthy life years (US$44m)
– Schizophrenia: 8,900 healthy life years (US$31m)
(3) Economic benefits of US$ 51 million are expected from depression treatment in Ethiopia as a result of productivity (equivalent to around 80% to the investment cost)
(4) Patients with mental health disorders in Ethiopia currently spend little money on mental health care in the statutory health system, simply because these services are not available. Universal public finance therefore averts little current private spending on health care and thus provides minimal financial risk protection.
Conclusion
The total mental and neurological package in Ethiopia is estimated to cost equivalent to US$1.8 per capita and yields large progressive health benefits. The expected productivity gain is substantially higher than the expected financial risk protection of universal public finance. The policy aims to provide essential mental health care in 50% of the over 3,000 primary health centres in Ethiopia. However, reaching patients with mental disorders is a challenge. Increasing coverage and to motivate patients to seek care will be crucial to achieve the ambitious policy targets in the mental health care strategy in Ethiopia. Future implications for other similar low income settings are that the Extended Cost Effectiveness Analysis approach seems to fit well with the mental health policy challenges and captures important equity implications of scaling up mental health care programmes.
—
The full article is available to view and download here: bit.ly/2eiqfkT
Image credit: Kjell Arne Johansson











