By: Allison Portnoy (Center for Health Decision Science, Harvard T.H. Chan School of Public Health)
What is financial risk protection?
Policymakers use a number of priority-setting frameworks to make decisions but accounting only for health gains and medical costs averted in the case of vaccination can neglect important questions of equity and financial burden on households. Financial risk protection is a key component of universal health coverage to ensure that all people have access to needed health services without financial hardship. Inherent in this goal is the concern of equity: in other words, who is and who is not protected against the financial hardship imposed by out-of-pocket medical payments—these high out-of-pocket medical expenses are referred to as ‘catastrophic health expenditures’ or CHE. Financial risk protection benefits indicate when an intervention or policy can reduce the number of cases of CHE experienced by households. Our approach incorporates financial risk protection into the economic evaluation of routine human papillomavirus (HPV) vaccination in Ethiopia to support cervical cancer prevention policy in this low-resource setting. This approach has already been used in practice to evaluate many different interventions in many different country contexts—generally resource-constrained settings where public finance of essential benefits, poverty reduction, and universal health coverage goals are especially relevant.
A look at Ethiopia and the burden of cervical cancer
Ethiopia is one of the largest countries in Africa and has one of the top ten growth rates in the world. Cervical cancer is the second leading cause of female cancer death in this setting. There are 32 million women over the age of 15 at risk of cervical cancer in Ethiopia, but preventive screening services for cervical cancer are extremely limited. Ethiopia is also very resource-constrained and more than one-third of health expenditures are financed by out-of-pocket payments. Cervical cancer can lead to a large financial burden on households due to the high cost of treatment. Public financing of the HPV vaccination has the potential to increase uptake of the vaccine and decrease mortality due to cervical cancer, but also can eliminate the incidence of these potentially large out-of-pocket expenditures associated with cervical cancer treatment. Given the size of the at-risk population and the further risk of CHE, priority setting in Ethiopia can be informed by examinations of financial risk protection across socioeconomic groups.
What did we find?
In our study we used a mathematical model that captures the main features of HPV vaccines and population demographics to project health and economic outcomes associated with routine HPV vaccination in Ethiopia. We estimated household out-of-pocket medical expenditures averted and cases of CHE averted. We assumed 100% vaccine protection against two specific cancer-causing HPV types and 50% vaccination coverage. Between 2019–2118, our analysis showed that routine HPV vaccination could:
- Avert up to 970,000 cases of cervical cancer
- Save approximately 932,000 lives
- Save households over $41.2 million in out-of-pocket medical expenditures
- Avert 33,900 cases of CHE
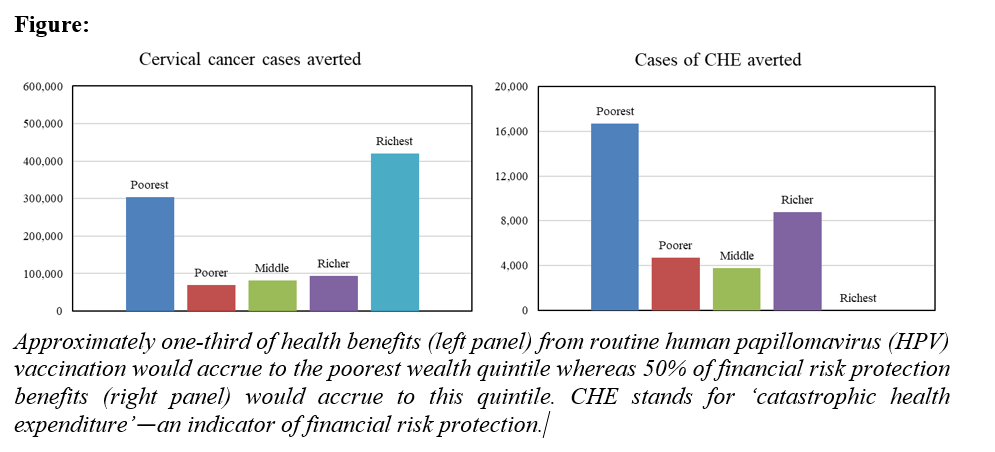
In the left panel of the figure below, you can see that the richest quintile experiences the greatest benefits followed by the poorest quintile with the second-greatest. This is due to assumptions that we made about the burden of cervical cancer and the rates of seeking treatment by household income level. Regardless, these distributions mean that approximately 30% of health benefits accrue to the poorest quintile. When we look at the financial risk protection benefits in the right panel of the figure, we can see that half (50%) of the financial risk protection benefits accrue to poorest quintile—this increase is due to the fact that the richest quintile does not experience CHE given the higher income levels of these households.
What does this mean?
In a resource-constrained setting with low screening coverage, HPV vaccination is vital for cervical cancer control efforts, and pro-poor policies are a vital contribution towards poverty reduction and universal health coverage goals. Our research attributes a reduction in disparities in cervical cancer incidence, mortality, and household health expenditures to routine HPV vaccination in Ethiopia. The pro-poor results of our study emphasize the potential equity-improving impact of routine HPV vaccination in cervical cancer control efforts. Including an examination of financial risk protection benefits can help policymakers with priority setting decisions regarding targeted investment in a routine HPV vaccination program. This analysis can inform fair and efficient priority setting in low- and middle-income countries with similar demographic and economic characteristics.
Related article:
Health gains and financial protection from human papillomavirus vaccination in Ethiopia: findings from a modelling study
Image credit: HPV Vaccination. With permission from Communications & Engagement at LSHTM











