John Peabody (University of California and QURE Healthcare) and David Paculdo (QURE Healthcare)
When governments look for ways to improve health care they grapple with questions of where and how best to spend scarce healthcare dollars. Urgency seems to take over effectiveness and they rarely ask what is the best return on spending. In analytic terms one of the big questions of our day is whether governments should invest more in enhancing access to care by expanding insurance coverage or invest in doctors to improve the quality of health care?
This is the research question we asked in the paper we recently published in Health Policy and Planning: “Comparative effectiveness of two disparate policies on child health: experimental evidence from the Philippines”.
We had an extraordinary opportunity to answer this question and to do so in a rigorous scientific way. We conducted a policy experiment in the Central Philippines, an area that covers one-third of the country, between 2003 and 2007. The experiment randomized whole communities into universal health coverage (UHC) versus pay-for-performance (P4P) versus usual policy and asked which intervention, compared to the controls, delivered the greatest improvement in patient outcomes for the lowest cost? At the beginning of the experiment, we measured the quality of care of doctors using our validated patient CPV vignettes.
In the UHC districts, coverage was provided to all children under the age of 5, under the guidance of Policy Navigators tasked with ensuring universal enrollment. In the P4P districts, providers were given personalized feedback based on care deficiencies identified by their performance on the patient vignettes. These providers participated in multiple serial rounds of vignette-based performance assessment and measurement, and were given bonus payments if their scores on the patient vignettes improved. Simultaneously, scores and coverage were tracked against the health of the population to determine the impact of the interventions against with real-world outcomes.
In our “comparative effectiveness” paper, we specifically looked at how well each policy reduced childhood wasting. Wasting is defined as low weight-for-height and is a sign of moderate malnutrition, that, according to the World Bank, has a prevalence of wasting among children under 5 of 7.42%. At baseline, we calculated that there were over three million disability-adjusted life years (DALYs) lost due to wasting in children younger than 5 in the Philippines – including 2.3 million years of life lost from more than 36,000 premature deaths per year.
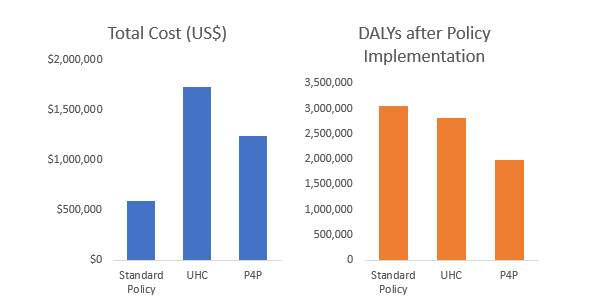
Each policy, whether it was insurance based UHC or doctor directed P4P, reduced wasting-related DALYs, and they did so to about the same degree. The P4P intervention, however, reduced these DALYs at a much lower cost. While UHC led to 330,000 fewer DALYs at US$7.03 each, P4P led to over one million fewer DALYs at US$4.29 each. The DALY decrease per US$ spent is 0.50 for UHC versus 1.52 for P4P, demonstrating a threefold greater effectiveness ratio for P4P. The DALY reduction under the P4P scheme may even be conservative, as secondary improvements due to higher overall quality delivery could not be measured.
Although this is a limited case scenario, reflecting only improvements in childhood wasting, the implications of these results are both unique and at a national scale. The uniqueness of making a simultaneous comparison at scale is a rare guidepost for health policy makers making large policy expenditures that can make a difference in thousands, if not millions, of lives.











