By: Professor Martin Antonio (LSHTM and WHO Collaborating Centre for New Vaccines Surveillance)
The global outbreak of novel coronavirus disease (renamed COVID-19) has brought to attention the preparedness of African countries and health systems to be able to address the COVID-19 outbreak. On 31 Jan 2020 the WHO Director-General, Dr Tedros Adhanom Ghebreyesus, declared the outbreak a public health emergency of international concern (PHEIC) and emphasised during this declaration that we are not yet aware of the damage this virus will do if it spreads to weaker health systems.
As of 24th Feb 2020, we know that there are an estimated 3-4,000 new cases being reported per day and 2,465 deaths globally with one death being reported in Egypt, Africa to date. The Africa CDC along with The MRC Unit The Gambia at the London School of Hygiene and Tropical Medicine (LSHTM) are building health capacity in Africa as part of health system strengthening efforts, including The MRC Unit The Gambia being the designated COVID-19 testing centre for The Gambia health services and in West Africa. We are employing the next generation whole genome sequencing as well as The Africa CDC’s real-time polymerase chain reaction (PCR) technique in order tounderstand the biology of the organism and help inform future vaccine design.
During the 2017 meningitis outbreak in Nigeria, some of the challenges facing Nigeria (and most of Africa) was health system strengthening and the importance of engaging policymakers to take heed of the outbreak. Once The MRC Unit The Gambia team had political support from the leaders of Nigeria, we were able to train the human health resources needed to contain the outbreak including health personnel (doctors, nurses, scientists, data managers etc.). We were also able to assist the ministry in financing the outbreak via WHO, UK Government and The MRC Unit The Gambia along with other partners. The information technology (IT) team were instrumental in ensuring that all the cases recruitment was linked to the disease. The medical supply team ensured vaccination kits, needles, reagents, fridges, freezers etc. were in place and successfully deployed.
For COVID-19 we need to similarly ensure strong leadership and governance as well as strengthening of the primary health care system to be able to prevent or at least adequately respond to future outbreaks within the community. For example, sharing appropriate standards of practice as well as deliverance of training are key. The utilisation of faith-based organisations to help spread these messages and social media messaging will also be vital within the region to increase public awareness and knowledge.
Conclusion
In conclusion, the case definition is of course different for COVID-19 in relation to other outbreaks but similar lessons can be learnt from previous outbreaks in terms of health systems strengthening and engaging policymakers. We will continue to work together with Africa CDC, WHO AFRO and The London School of Hygiene & Tropical Medicine to prepare Africa and our health systems in the event of an outbreak.
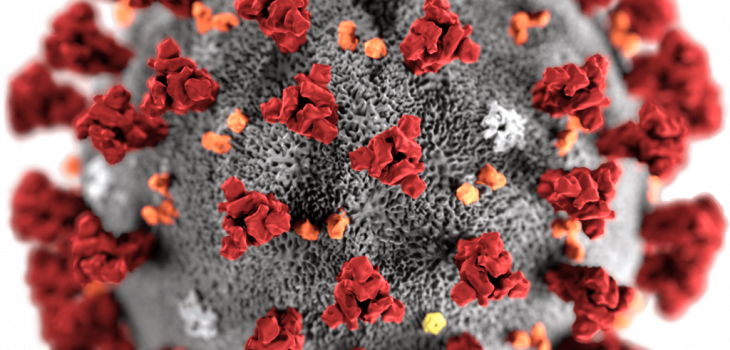
Image credit: CDC/ Alissa Eckert, MS; Dan Higgins, MAM – This media comes from the Centers for Disease Control and Prevention‘s Public Health Image Library (PHIL), with identification number #23312.
This illustration, created at the Centers for Disease Control and Prevention (CDC), reveals ultrastructural morphology exhibited by coronaviruses. Note the spikes that adorn the outer surface of the virus, which impart the look of a corona surrounding the virion, when viewed electron microscopically. A novel coronavirus, named Severe Acute Respiratory Syndrome coronavirus 2 (SARS-CoV-2), was identified as the cause of an outbreak of respiratory illness first detected in Wuhan, China in 2019. The illness caused by this virus has been named coronavirus disease 2019 (COVID-19).